.
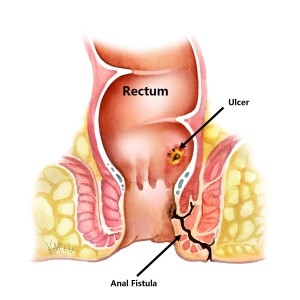
An anal fistula is a communicating tract between the inner anus or rectum and the external skin surrounding the anus. It begins as a superficial ulcer (Figure 1), that becomes infected creating an anal abscess that subsequently bursts leaving a communicating tract between the internal anus and the external skin of the perianal region. It causes a chronic discharge of pus that typically has an offensive odour.
Types
A perianal fistula can be short and superficial, not involving the anal sphincter (submucosal fistula) or can be long and deep, involving the just the internal anal sphincter (intersphincteric fistula) or both anal sphincters (transphincteric fistula or extrasphincteric). Most fistulae are low arising from low within the anal canal. Rarely fistulas are high, arising from above the anal canal (supralevator fistula).
Simple fistulae
Simple fistulae are those with a single tract that involves less than 30-50% of the external anal sphincter. The preferred treatment of a simple fistula is to lay it open [1]. This is a small operation under general anaesthetic, in which a probe is placed in the fistula, and the overlying skin cut to allow the tract to heal as a shallow ulcer.
Complex fistulae
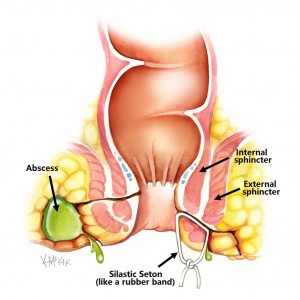
Complex fistulae, are those with multiple tracts, those that involve more than 30-50% of the external sphincter, those that involve the anterior half of the anus (in women), any fistula as a result of radiation or Crohn’s disease, and those arising in someone with already compromised sphincter function (i.e. weak anal tone prone to incontinence). These cannot simply be laid open, and often the first step is to control the sepsis by inserting a seton (figure 2).
Cause
Anal fistulae result when an anal abscess bursts into the tissues surrounding the anus. This condition is common in young adults, but can occur at any age. The reason why some people develop a fistula, and others don’t is not known. Smoking and Crohn’s disease have both been shown to increase your risk of developing a fistula. The success of surgery for the treatment of fistulae due to Crohn’s disease or in the smoker is considerably lower than for other fistulas. Infliximab infusions have been shown to increase the success of fistula closure in Crohn’s disease [2].
Symptoms
A chronic discharge of malodourous pus from the perianal region is the usual feature of an anal fistula. This is often followed a period of intense perianal pain that coincides with the time of abscess formation.
Investigation
The diagnosis is made clinically, and confirmed by an Examination Under Anaesthesia (EUA), where a probe is gently inserted into the fistula tract to confirm a communication between the outside perianal skin and the internal lining of the anal canal. Occasionally Endo Anal Ultrasound (EAU) or Magnetic Resonance Imaging (MRI) are needed to determine the number and direction of fistula tracts, and to determine the amount of muscle sphincter involved prior to any planned surgery.
Course
The initial management of a fistula is to drain it. This is a small surgical procedure performed under general anaesthetic where a silastic seton (similar in size and consistency to a rubber band) is passed through the fistula tract and tied in place. This allows any pus to drain, and inflammation to settle. A course of antibiotics may also be required.
Simple fistulae
Within 6 weeks, the condition should be much improved, and you will need to be re-examined by a colorectal surgeon to determine if the internal opening of the fistula is low (and safe to lay open) or not. This is a simply procedure where a Lockhart Mummery probe is passed through the fistula tract and using diathermy, the roof of the tract incised turning the fistula tract into an ulcer. This will slowly heal over 6-12 weeks.
If the internal opening of the fistula tract is high, it involves too much of the internal sphincter, and it is not safe to incise, as loss of this vital muscle will result in incontinence. Therefore, at this point there are 4 options:
- Remove the seton;
- Tighten the seton (repeated every 6-12 weeks);
- Remove the seton and use glue or a plug to seal the tract;
- Leave the seton in place for 6 months to allow “maturing” of the fistula tract prior to planned surgical repair.
Remove the seton
If the seton has been in for only 6 weeks, and the infection has settled, simply removing the seton has been shown to be effective in up to 75-80% of cases [3,4]. The success following simple removal of the seton is reduced to less than 50-60% for patients with Crohn’s disease [5]
Tighten the seton
Sequential tightening of the seton under anaesthetic every 6-12 weeks leads to the seton eventually cutting through the muscle sphincter. Because the cutting process is very slow, it allows scar tissue to form between the cut ends of the sphincter muscle, allowing the circular sphincter muscle to still function as a sphincter. This whole process can take anywhere from 3-12 months to complete.
Remove the seton and use glue or a plug to seal the tract
A vast number of plugs and glues have been used to try to seal fistula tracts. The argued benefit of these techniques is that they preserve the anal sphincters. Several products are commercially available and treatment involves single or repeated injection into the external opening. Initial studies were promising with healing rates of up to 70% with no studies reporting impairment of continence[7]. However more recent studies looking at long-term healing rates show disappointing recurrence rates as high as 75%. [8-10]. Therefore, a selective approach is recommended, with only some fistulae suitable for plugs. There is some evidence suggesting that long tracts greater than 4cm in length are more likely than short tracts to heal with these techniques [11].
Leave the seton in place for 6 months to allow “maturing” of the fistula tract prior to planned surgical excision and repair.
If the fistula tract is high, it is unsafe to cut the anal sphincter, and the seton is left in place for 6 months to allow the fistula tract to “mature”, with epithelialization of the tract occurring. Once this maturation process has occurred, a surgical repair can then be performed. This may involve simple ligation and excision of a portion of the fistula tract, without the use of a flap (i.e. LIFT procedure) or may involve excision of the entire length of fistula tract followed by a formal flap repair to cover the internal opening.
If the internal opening is very high in the anal canal a rectal advancement flap is performed using a flap of mucosa and the underlying muscle to cover the internal opening. If the internal opening is low enough in the anal canal, an anoderm V-Y advancement flap may be preferable. Both these flap repairs also involve repairing the sphincter, and usually result in the external opening remaining open to allow for drainage.
What to expect pre and post operatively following anal fistula surgery
Fasting and Bowel Preparation
Unless you are also having a colonoscopy, a normal diet without bowel preparation, is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 7am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 90 and 60 minutes prior to your operation.
Recovery and transport
Following your procedure, you will recover for an hour until the effects of sedatives have worn off. You should not drive yourself home after your procedure and should have someone organised to accompany you home.
Bleeding
Spotting of blood or persistent minor oozing will occur for 5 days and a sanitary napkin changed once to twice daily will be needed to prevent staining. Bleeding will typically occur after opening your bowels. If the bleeding is more than a couple of teaspoons a day, notify your surgeon.
Laxatives
A tablespoon of natural psyllium husk (Metamucil® or Fibogel®) three times daily is recommended the first 2 weeks after surgery
Pain control
A non-steroidal is recommended such as 400mg of ibuprofen (Brufen®) along with 2 tablets of paracetamol up to three times a day. Opioid medications (Endone) may sometimes be needed, but should be used sparingly as they cause constipation.
Antibiotics
You may require antibiotics to treat ongoing infection. Oral Augmentin Duo Forte® twice daily (if not allergic to penicillin) for 5 days is adequate. Otherwise cephazolon (Keflex®) &metronidazole (Flagyl®).
Dressings
A simple pad is all that is usually required, changed twice daily.
Sitz baths
Twice daily warm to hot salt water (Sitz) bathing to the anal region is soothing and antiseptic, and should be done for 1 -2 weeks following your procedure. Put a handful of salt into a shallow bath of warm-to-hot water and sit there for 10-30 minutes.
Follow-up
You should follow up with your colorectal surgeon in 6 weeks following your surgery to review your wound and discuss further management if indicated.
References
- Williams JG, Farrands PA, Williams AB, Taylor BA, Lunniss PJ, Sagar PM, Varma JS, George BD. The Treatment of Anal Fistula: ACPGBI Position Statement. Colorectal Disease. 9 (Suppl. 4): 18-50, 2007.
- Sands B, Anderson F, Bernstein C, Chey W, Feagan B, Fedorak R, Kamm M, Korzenik J, Lashner B, Onken J, Rachmilewitz D, Rutgeerts P, Wild G, Wolf D, Marsters P, Travers S, Blank M, van Deventer S. Infliximab maintenance therapy for fistulizing Crohn’s disease. The New England Journal of Medicine New England Journal of Medicine. 350 (9): 876–85, 2004.
- Joy HA, Williams JG. The outcome of surgery for complex anal fistulas. Colorectal Disease. 4: 254-61, 2002.
- Eitan A, Koliada M, Bickel A, et al. The use of the loose seton technique as a definitive treatment for recurrent and persistent high trans-sphincteric anal fistulas: a long-term outcome. Journal of Gastrointestinal Surgery 2009; 13(6):1116-9.
- Faucheron JL, Saint-Marc O, Guibert L, et al. Long-term seton drainage for high anal fistulas in Crohn’s disease–a sphincter-saving operation? Diseases of the Colon & Rectum 1996; 39(2):208-11.
- Lentner A. Wienert V. Long-term, indwelling setons for low transsphincteric and intersphincteric anal fistulas. Experience with 108 cases. Diseases of the Colon & Rectum. 39(10):1097-101, 1996 Oct.
- Johnson E, Gaw J, Armstrong D. Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Diseases of the Colon and Rectum 49(3): 371-6, 2006.
- Buchanan G, Bartram C, Phillips R, etal. The efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial. Diseases of the Colon and Rectum. 46: 1167-74, 2003.9. van Koperen PJ. Bemelman WA. Gerhards MF. Janssen LW. van Tets WF. van Dalsen AD. Slors JF. The anal fistula plug treatment compared with the mucosal advancement flap for cryptoglandular high transsphincteric perianal fistula: a double-blinded multicenter randomized trial. Diseases of the Colon & Rectum. 54(4):387-93, 2011 Apr.
- Ortiz H, Marzo J, Ciga MA, Oteiza F, Armendariz P, de Miguel M. Randomized clinical trial of anal fistula plug versus endorectal advancement flap for the treatment of high cryptoglandular fistula in ano. Br J Surg. 2009;96:608–612.
- McGee MF. Champagne BJ. Stulberg JJ. Reynolds H. Marderstein E. Delaney CP. Tract length predicts successful closure with anal fistula plug in cryptoglandular fistulas. Diseases of the Colon & Rectum. 53(8):1116-20, 2010 Aug.