.
Bowel cancer is the second commonest cancer in Australia. Most colorectal cancer, if picked up early, can be cured with surgery alone, with a better prognosis than most other cancers.
Cause
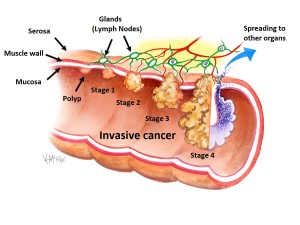
Most colorectal cancers originate from a polyp. A series of step-wise mutations leads over several years to a polyp becoming a cancer (figure 1). As the cancer gets bigger, it invades the muscle layer of the bowel wall, then the other lining (serosa) before spreading to the nearby glands (lymph nodes) (figure 1). The aim of colonoscopy is to allow these polyps to be removed before they become cancer.
Most of these mutations occur sporadically, with inherited genetic syndromes such as Familial Adenomatous Polyposis (FAP) and Lynch Syndrome, also called Hereditary Non Polyposis Colorectal Cancer (HNPCC) accounting for less than 6% of all colorectal cancers. The main risk factors for colorectal cancer include a family history of colorectal cancer, previous polyps, and age greater than 50. Other risk factors include obesity, smoking, excessive alcohol intake, lack of fruit and vegetables and fibre in the diet, and excessive ingestion of meat and animal fats.
Symptoms
Colon cancers rarely cause symptoms until very late. Rectal cancers may result in bleeding, and can be mistaken for haemorrhoids. Rectal cancers may also cause rectal pain on straining or urgency to defecate (tenesmus). All cancers, if large enough, can cause obstruction, with abdominal bloating and pain very similar to that experienced from constipation.
Investigations
Any patient with a family history of colorectal cancer, previous polyps, rectal bleeding, or change in bowel habit should visit their colorectal surgeon to discuss having a colonoscopy to view the entire colon and rectum. If a colorectal cancer is found at colonoscopy, it is biopsied to confirm that it is in fact a cancer. Prior to surgery, a CT scan of the abdomen and pelvis should be performed to show the size of the tumour and to exclude spread of the cancer elsewhere. Occasionally a PET CT is also required to rule out distant spread (metastases).
Course
Colorectal cancer, if picked up early before it has broken through the bowel wall (Stage I-II), is cured with surgery alone. If it has spread to the lymph nodes (Stage III), it can be cured with a combination of surgery and chemotherapy. Colorectal cancers if treated aggressively with surgery frequently do better than other cancers. If your colorectal cancer has already metastasised to liver, bones or lung, you should discuss with your GP whether or not a referral to a colorectal surgeon is indicated, as there may still be a role for surgery in combination with chemotherapy and/or radiotherapy.
Prevention
A healthy lifestyle, consisting of regular exercise, a diet rich in fruit and vegetables and fibre, and the avoidance of smoking, excessive alcohol, meat and animal fat intake, can all help reduce your risk of colorectal cancer.
Those at high risk of colorectal cancer should have regular screening colonoscopy at least every 3-5 years, with removal of polyps when they are still small.
Those with rare inherited genetic syndromes (HNPCC and FAP) should speak with their colorectal surgeon and geneticist to discuss the role of preventative (prophylactic) colectomy.
Medical management
The primary treatment of colorectal cancer is surgery. However, occasionally, the tumour is large or there is spread of cancer to or beyond lymph nodes. In these situations, radiotherapy and/or chemotherapy may be also indicated. Occasionally chemotherapy is given on its own in a palliative setting when there is widespread cancer metastasis. All colorectal cancer cases are discussed in a Multi-Disciplinary Team (MDT) meetings with expert colorectal surgeons, radiologists and medical and radiation oncologists.
Endoscopic surgery for early bowel cancer
Endoscopic surgery is sometimes indicated for very early cancer, such as the malignant polyp. It can also be indicated for the elderly or frail where major surgery would carry unacceptably high risk. In most cases however, formal surgery with resection of a section of bowel (colectomy) . This removes the cancer as well as the glands (lymph nodes) that the cancer can potentially drain to. The two ends of healthy bowel are then joined together creating an anastomosis (figure
What to expect post operatively after endoscopic surgery for colorectal surgery
Diet
Immediately after your procedure you will be commenced on free fluids (semi thickened fluids such as custard, yoghurt, thin porridge). You will be commenced on a light diet once you have passed flatus. You will be discharged from hospital eiyther the same day or the following day after your endoscopic procedure.
Activity
You will be up and mobilising from day one and able to conduct most actitivities from day one.
Length of stay
Endoscopic removal of a malignant polyp or early bowel cancer can usually be done as day stay, although sometimes overnight admission is required.
Post operatively, you will need to see your colorectal surgeon at 3-6 weeks post-operatively to check on you progress.
Follow-up and appointments
You will then be followed up regularly (every 1-3 years), with colonoscopy performed at regular intervals.