.
Crohn’s disease, is an inflammatory bowel disease (IBD) that may affect any part of the gastrointestinal tract (GIT) from mouth to anus, causing a wide variety of symptoms. It primarily causes abdominal pain, diarrhoea (which can be bloody when inflammation is uncontrolled), vomiting, and can also cause complications outside the GIT such as skin rashes, arthritis, inflammation of the eyes, and hepatitis.
Risk factors for Crohn’s disease
The exact cause of Crohn’s disease is not known, with many factors likely to be responsible. In part, it is thought to be autoimmune in origin, with the body’s immune system attacking the GIT, causing inflammation. There is also evidence of a genetic link to Crohn’s disease with siblings of those with Crohn’s disease at higher risk. Environmental factors are also likely to be responsible as evidenced by the higher incidence in Western industrialized nations. This is likely to be in part due to the increased consumption of processed foods. Smokers are twice as likely to develop Crohn’s disease than non-smokers.
Incidence
Crohn’s disease is an important cause of morbidity in Australia, with a prevalence of about 50 per 100 000 population. It has a bimodal peak, occurring most commonly in young adulthood, with a second smaller peak in the sixties.
Is there a cure for Crohn’s disease?
There is no known medical or surgical cure for Crohn’s disease. Treatment is aimed at controlling the disease and symptoms, maintaining remission, and preventing relapse. Surgery has a role for disease that is resistant to medical treatment.
Types of Crohn’s disease
Broadly speaking Crohn’s disease is of three types:
- inflammatory type in which there is inflammation of the intestine with diarrhoea, sometimes bloody;
- stricturing type, in which there is scarring and fibrosis of the intestine leading to obstruction with crampy abdominal pain; and
- fistulising type in which abnormal channels or tracts form between adjacent loops of bowel, or even between bowel and the skin. Oftentimes, the three types co-exist to some extent.
Site of disease
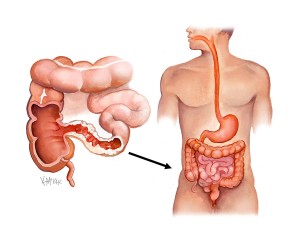
Crohn’s disease can attack any part of the digestive tract, from mouth to the anus. However, as a general rule, most individuals affected by Crohn’s disease fall into 3 categories:
- ileocolic Crohn’s affects both the ileum (the last part of the small intestine, which connects to the large intestine), and the large intestine and accounts for up to 50% of cases;
- Crohn’s ileitis, affects only the ileum, and accounts for 30% of cases (fig 1); and
- Crohn’s colitis affects only the large intestine and is responsible in 20% of cases and may be difficult to distinguish from another form of IBD called ulcerative colitis. Crohn’s disease of the stomach and first part of the small intestine (duodenum and jejunum) can occur although is uncommon.
Appearance of Crohn’s disease from the inside
All patients with suspected Crohn’s disease require a gastroscopy and a colonoscopy to visualise the inside of the intestine and stomach. The typical features of Crohn’s disease are inflammation of the intestine, with sometimes bleeding of its mucosal lining. In severe cases, long thin, almost snake-like (serpiginous) ulcers can be seen. Occasionally, these ulcers are so large that they begin to coalesce, resulting in only small islands of normal tissue which are referred to as ‘psuedopolyps’.
How is Crohn’s disease different from ulcerative colitis?
Crohn’s disease is distinguished from ulcerative colitis by the presence of ‘skip-lesions’ where there are two or more areas of diseased bowel with normal healthy bowel intervening. Crohn’s disease can also affect any of the GIT from mouth-to-anus, whereas ulcerative colitis only affects the large intestine, and always begins at the rectum with confluent involvement. If disease is seen in the small intestine, or if disease is seen in the large intestine and the rectum is not involved, or if disease is not confluent with ‘skip lesions’, then it is probably not ulcerative colitis. Also biopsies will be performed at the time of colonoscopy, with microscopic examination of the specimen. In Crohn’s disease, this will typically show inflammatory white blood cells (lymphocytes) throughout the whole thickness of the bowel. In contrast ulcerative colitis typically only involves the inner part of the bowel wall. In 50% of Crohn’s patients fused giant chronic inflammatory cells (granulomas) are present, and their presence helps to clinch the diagnosis.
Difficulties making the diagnosis of Crohn’s disease
Many patients with Crohn’s disease often had symptoms that pre-dated their diagnosis by many years. The usual onset of Crohn’s disease is between 15 and 30 years of age, but can occur at any age. Because of the ‘patchy’ nature of the disease, initial symptoms can be more subtle than those of ulcerative colitis. Crohn’s disease also tends to “wax and wane’ and people with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. This may lead many to defer investigation of their symptoms as they appear to get better during their remission phase.
Confirming Crohn’s disease requires colonoscopy with tissue biopsy. Frequently the features on biopsy are not strong enough to make a firm diagnosis of Crohn’s disease, as the classic feature is the formation of granulomas, which is absent in up to 50% of acute episodes.
Common symptoms of Crohn’s disease
Abdominal pain may be the initial symptom of Crohn’s disease. Diarrhoea may also coexist, or be the only symptom. The diarrhoea sometimes contains mucous and blood. Flatulence and bloating may also add to the intestinal discomfort. Crohn’s patients can experience mouth discomfort due to mouth ulcers, or pain, discharge or itching from the anus due to the development of an anal abscess or anal fistula.
Extra-intestinal signs of Crohn’s disease
The non-intestinal complications of Crohn’s disease may also occur. Occasionally hepatitis or yellow skin (jaundice) can result from inflammation and blockage of the drainage ducts (bile ducts) of the liver due to primary sclerosing cholangitis. Red rashes on the skin (erythema nodosum) on the back or palms of hands may occur. In extreme cases, these can become pussy ulcers, usually on the shins of the legs. This is often a sign of poorly control intestinal Crohn’s disease. Inflammation of the interior portion of the eye, known as uveitis, can cause eye pain, especially when exposed to light (photophobia). Inflammation of the white part of the eye with redness can occur and is a condition called episcleritis. Inflammation of one or more joints (arthritis) can occur. Typically, the arthritis can affect larger joints, such as the knee or shoulder, or may exclusively involve the small joints of the hands and feet. The arthritis may also involve the entire spine (ankylosing spondylitis) or simply the lower spine (sacroiliitis). The symptoms of arthritis include painful, warm, swollen, stiff joints and loss of joint mobility or function. This form of arthritis is said to be ‘sero-negative’, as they usually do not have the rheumatoid factor seen in a blood test for rheumatoid arthritis.
Complications of untreated Crohn’s disease
Crohn’s disease can lead to several mechanical complications within the intestines, including obstruction, fistulae, and abscesses. Obstruction typically occurs from strictures or adhesions that narrow the lumen of the intestine. Fistulae can develop between two loops of bowel, between the bowel and bladder, between the bowel and vagina, and between the bowel and skin. Abscesses are walled off collections of infection, which can occur in the abdomen or in the perianal area (anal abscess) in Crohn’s disease sufferers.
Crohn’s disease and bowel cancer
Crohn’s disease also increases the risk of bowel cancer in the area of inflammation. The greater the area of inflammation, the greater the risk of cancer. The life-time risk of colorectal cancer in the normal population is 1 in 12. In patients with Crohn’s colitis involving their entire large their lifetime risk is 5.6 times higher that of the normal population. This means that their lifetime risk of developing colorectal cancer is almost 50%. Screening colonoscopy for colon cancer is recommended for anyone who has had Crohn’s colitis for at least eight years. Folate and mesalamine (Pentasa®) may help to reduce the risk of colorectal cancer.
Fertility and Crohn’s disease
Reduced fertility can result from poorly controlled Crohn’s disease.
Pregnancy and Crohn’s disease
Crohn’s disease can be problematic during pregnancy, and some medications can cause adverse outcomes for the foetus or mother. Consultation with your obstetrician about Crohn’s disease and all medications allows preventative measures to be taken.
Genetics
Crohn’s disease runs in families and those with a sibling with the disease 30 times more likely to develop it than the general population. Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn’s disease. It is now known that over 30 genes play a role in the disease. Abnormalities in the XBP1 gene have recently been identified.
Environmental factors
The industrialised diet that consists of heavily over-processed foods, is believed to be linked to the higher prevalence of Crohn’s in the Western world. Smoking has been shown to increase the risk of a flare up of Crohn’s disease.
Immune system
Crohn’s disease is partly thought to be an autoimmune disease. The overproduction of various chemicals (cytokines) release by a special class of white blood cells called T helper cells, is seen in Crohn’s disease.
Infective cause
Some studies have suggested that Mycobacterium Avium Paratuberculosis (MAP) plays a role in Crohn’s disease, as its infection causes very similar disease (Johne’s disease) in cattle. However subsequent studies have casted considerable doubt on this theory.
Colonoscopy and gastroscopy for Crohn’s disease
A colonoscopy is the best test for making the diagnosis of Crohn’s disease, as it allows direct visualization of the colon and the terminal ileum, identifying the pattern of disease involvement whilst also allowing for biopsies to be taken. These biopsies are sent for laboratory analysis, which may help confirm the diagnosis. As 30% of Crohn’s disease involves only the ileum, cannulation of the last bit of small bowel before it enters the large bowel (terminal ileum) at the time of colonoscopy, is required. Gastroscopy allows visualisation of the stoma and duodenum. Occasionally the gastroscope can travel past the duodenum into the jejunum, allowing for this to be examined and biopsied as well.
Other methods for assessing small bowel
Because colonoscopy and gastroscopy only allow direct visualization of the large bowel, terminal ileum and duodenum with occasional views of the jejunum, other methods are sometimes needed to see the intervening small bowel (jejunum and ileum) that cannot be reached with a scope.
Small bowel enteroclysis
Small bowel enteroclysis, involves a CT scan of the abdomen with the ingestion of large volumes of water to distend the small bowel. This will allow for CT reconstructions that give a view of what the inside of the small intestine looks like. It is useful for seeing if narrowing (strictures) or thickenings in the bowel are present.
Pill CAM
Pill CAM, involves the ingestion of a large capsule which contains a camera within it. It takes a series of photos as it passes through the small intestine, and can help show the inside of the intestine (jejunum and ileum) that cannot be reached at gastroscopy and colonoscopy. It should not be used in patients in whom obstruction or blockage is suspected. If there is doubt, a dissolvable ‘dummy’ capsule should first be used, and if this passes through without blockage, then it is safe to swallow a pill-cam.
Blood tests
Acute exacerbations of Crohn’s disease are invariably associated with raised inflammatory markers, which include a raised white cell count (WCC), erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP). Chronic malnutrition and failed absorption of iron and vitamin B12 from the terminal ileum may also be revealed by blood tests which show a reduced albumen level, lymphocyte count, and haemoglobin. Testing for Saccharomyces cerevisiae antibodies (ASCA) and anti-neutrophil cytoplasmic antibodies (ANCA) can help differentiate Crohn’s disease from ulcerative colitis.
Aim of management of Crohn’s disease
There is currently no cure for Crohn’s disease with the aim of treatment to induce remission. Remission may not be possible or prolonged if achieved. In such cases, surgery may be indicated. In cases where remission is possible, relapse can be prevented and symptoms controlled with medication, lifestyle changes, and, in some cases, surgery.
Lifestyle modification
Lifestyle changes may include dietary modification with the adoption of an elemental diet, or low residue diet with small frequent meals during acute attacks, and inclusion of all food groups to avoid against vitamin or protein deficiencies. Occasionally vitamin supplementation is needed. Foods known to trigger an attack should be avoided, and a food diary may help determine which foods do this. In some patients milk or dairy products can trigger an attack, but this is not a consistent finding. Smoking cessation has been shown to reduce attacks. Regular exercise can help combat chronic fatigue.
Medication
Medical treatment is aimed at treating any infection with antibiotics reducing inflammation with anti-inflammatories such as aminosalicylates and corticosteroids). When Crohn’s is in remission, treatment is aimed at maintenance and the avoidance of recurrence of symptoms. Your gastroenterologist is important in deciding the right medical treatment regimen for you.
Medications used to treat the symptoms of Crohn’s disease include 5-aminosalicylic acid (5-ASA) formulations, prednisone, immunomodulators such as azathioprine (Imuran®), mercaptopurine and methotrexate.
A new class of biologics which are tumour nercrosis factor (TNF) inhibitors and require intravenous infusion include infliximab (Remicade®), adalimumab (Humeria®), certolizumab (Cimzia®) and natalizumab (Tysabri®).
Intravenous hydrocortisone should be used in severe attacks of Crohn’s disease, which is then converted to oral prednisone, and tapered with the aim of eventually eliminating its use once disease activity is controlled.
Side effects of medication
Prolonged use of corticosteroids has significant side-effects. As a result, they are in general not used for long-term treatment. Alternatives include aminosalicylates alone, though only a minority are able to maintain the treatment, and many require immunosuppressive drugs. It has been also suggested that antibiotics change the enteric flora, and their continuous use may pose the risk of overgrowth with pathogens such as Clostridium Difficile. Long-term use of metronidazole (Flagyl®) can also lead to neuropathy.
Surgery for Crohn’s disease
Surgery does not cure Crohn’s disease, but corrects an immediate problem that cannot be resolved using medication. Five types of surgery are commonly performed on individuals with Crohn’s disease:
- Partial bowel resection (to remove a diseased portion of intestine)
- Strictureplasty (to widen an area of narrowed intestine)
- Correction of fistulas
- Draining of an abscess
- Preventative total colectomy for Crohn’s pancolitis
It is estimated that about 75% of individuals who live with Crohn’s disease will require surgery at some point in their lives.
Partial bowel resection
Resection is usually performed when a portion of intestine has been so damaged by disease that a permanent partial obstruction has formed. The most common areas removed are the terminal ileum, the ileocaecal valve, and a small portion of the large intestine. During this surgery, your colorectal surgeon will attach (anastomose) the healthy ends of intestine together with a special stapling device. Sometimes, however, there is mild inflammation throughout the intestine, preventing such reattachment. In these cases, a temporary stoma is created. The stoma allows intestinal contents to drain directly out of the body into a collecting bag through the abdominal wall. The stoma is usually closed and the bowel reattached 8-12 weeks after the initial surgery. Occasionally, permanent stomas are required.
After surgery, disease may occur above the surgical point, closer to the stomach and further resections are sometimes necessary. Research shows that some of the new 5-ASA compounds such as mesalamine (Pentasa®) are helpful in delaying the recurrence of symptoms after surgery.
Stricturoplasty
Endoscopic strictureplasty is a procedure that opens up small narrowings (strictures) in the bowel. An incision is made down the length of stricture. The incision is pulled together and sewn across the stricture, shortening the intestine slightly but widening the formerly narrowed area.
Correcting fistulas
Fistulas that connect the intestine to another internal organ, such as the bladder, must be surgically closed in order to keep intestinal contents from draining into the organ and causing infection.
Draining abscesses
When an abscess does not respond to medical treatment, it must be drained to promote healing. Needle aspiration is the most common method. A hollow needle is inserted through the skin and into the abscess, then used to withdraw the infectious material. In another method, a surgeon exposes the abscess surgically, removes the infectious material, and places a wick to promote drainage and healing from the inside.
Surgery
Surgery is usually a last resort option, but is occasionally needed. Patients with Crohn’s disease affecting their colon, have an increased risk of developing colorectal cancer, and should have regular colonoscopies every 3-5 years. The risk is greatest in those with most of their colon involved (pancolitis). Early changes that suggest a risk of developing cancer include the development of dysplasia. This progresses from mild to moderate to high grade dysplasia over time, before becoming invasive cancer. In those with high grade dysplasia or colorectal cancer, removal of the entire large bowel may be indicated, because of the very high risk of developing subsequent cancers if the colon is not removed.