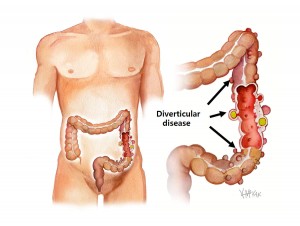
Diverticular disease of the colon is where “pockets” occur at weaknesses in the colon wall. These pockets are called diverticula. These pockets typically occur in the last part of the colon before reaching the rectum (the sigmoid colon). When one or more of these diverticula rupture it results in inflammation or infection of the involved colon (diverticulitis).
Cause
Age and constipation are the leading causes of diverticular disease.
Constipation results in the colon needing to generate very high pressures to squeeze the firm faeces along the colon. These high pressures result in “blowouts” with pockets or pouches (called diverticula) in the wall of the colon at weaknesses in the muscle wall where the blood vessels enter. When a diverticulum ruptures (even if microscopic), it leads to inflammation and infection of the involved colon (diverticulitis). If the diverticulum erodes into an adjacent blood vessel, it can result in bleeding into the colon.
Symptoms
Frequently diverticular disease is not associated with symptoms. However, when there is inflammation or infection (diverticulitis), this may result in abdominal pain and fevers. Per rectal bleeding can occur with diverticular disease when the diverticula is wide and causes mucosal erosion into an adjacent vessel. It is rare for diverticulitis and bleeding to occur together.
Investigation
Frequently diverticulosis is present without symptoms and the diagnosis is picked up by chance on colonoscopy or on gastrografin enema.
If the presentation is abdominal pain and fever consistent with diverticulitis, then a CT scan will confirm the diagnosis showing a swollen inflamed colon with associated diverticulosis. If the presentation is rectal bleeding a CT angiogram may be needed to determine that it is diverticular bleeding. This will also tell the site of bleeding.
Course
Most cases of diverticular disease will never become symptomatic, with attacks of diverticulitis or per rectal bleeding very uncommon. Diverticulitis usually settles with antibiotics. Repeated attacks of diverticulitis are worrying and you should consult your colorectal surgeon to discuss the role of prophylactic surgery.
Diverticular bleeding is also uncommon, but when it occurs can result in significant per rectal bleeding, and warrants admission to hospital. Sometimes the bleeding must be stopped by injecting an agent (thrombin) via a groin artery (angiography) into the bleeding vessel (embolisation). Even more rarely emergency surgery is required to stop diverticular bleeding.
Prevention
A healthy diet high in fibre and a good intake of fluid to prevent dehydration and constipation is the best way to avoid diverticular disease. Constipation is sometimes resistant to dietary methods alone. Laxatives that prevent constipation include those containing psyllium husks (Metamucil®, Fibogel®), lactulose (Duphulac®), and sterculia (Normacol®). Attacks of diverticulitis are occasionally triggered by certain foods (e.g. nuts) however the evidence for this is weak.
Medical management
Diverticulitis with inflammation or infection of the affected colon usually settles with intravenous antibiotics, followed by an extended course of oral antibiotics following discharge from hospital. Diverticular bleeding is an indication for admission to hospital, but in most cases stops without treatment and only rarely requires embolisation or surgery.
Surgical management
In most cases surgery can be avoided, but recurrent attacks of diverticulitis warrant discussion with your colorectal surgeon about the benefits of prophylactic surgery.