.
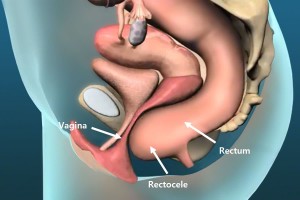
A rectocele results when the rectum bulges on straining, resulting in failed evacuation of stool (fig 1). It is more common in women, and typically the bulge is at the front (anteriorly) into the vagina. It leads to incomplete evacuation of the rectum on straining, and can be a cause of constipation.
Symptoms
The main symptom is incomplete evacuation of the rectum on straining. Frequently, this leads to the feeling that one needs to evacuate again soon after the last attempt. This feeling can at times be so overwhelming, that a compulsion to digitally evacuate the rectum is felt.
Diagnosis
The diagnosis is based on the presence of classic symptoms, the confirmation of an anterior bulge in the rectum on clinical examination and on defecating proctogram, a real-time x-ray taken while defecating. Anal physiology tests including manometry typically show reduced rectal pressures and increased compliance of the rectum.
Medical management of a rectocele
The maintenance of a soft stool consistency is important in preventing constipation and overdistension of an easily distensible rectum. Regular fibre, including a tablespoon of metamucil® twice a day, and 30ml of lactulose (Duphulac®) either once or twice a day may be needed.
Surgical management of a rectocele
A rectocele repair is occasionally indicated. Perineal approaches from below repair the defect via an incision made in the anterior wall of the rectum. Key hole abdominal procedures such as ventral mesh rectopexy, correct the underlying cause, by improving the suspension of the rectum and pelvic floor.
Perineal rectocele repair
This is a day stay procedure. It involves raising a flap of mucosa to gain access to the weakened part of the wall of the rectum at the front (anteriorly) and gathering up the muscles in this area with a series of reinforcing sutures, before closing the flap over the repair.
Laparoscopic ventral rectopexy (LVR)
Laparoscopic ventral rectopexy (LVR) is a procedure where the septum between the vagina and rectum is mobilised to the pelvic floor, with a piece of bio-dissolvable collagen mesh sutured to the pelvic floor and front wall of the rectum and anchored to the sacral promontory to lift the rectum back up in its normal place. Increasingly Robotic Ventral Mesh Rectopexy is being performed utilising da Vinci® technology.
What to expect pre and post operatively for rectocele surgery
Unless you are also having a colonoscopy, a normal diet without a bowel prep is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 6am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 90 minutes and 60 minutes prior to your rectocele operation.
Following your procedure, you will recover for a hour until the effects of sedatives have worn off. Typically, an overnight admission is required for perineal repairs, and a 2-3 day admission for ventral mesh rectopexy.
You should remain on regular laxatives and simple analgesics for 1 week. We recommend taking twice daily a tablespoon of natural psyllium husk (Metamucil® or Fibogel®), and 30ml of lactulose (Duphalac®) daily or twice daily to keep stool consistency soft. For pain we recommend after each meal 400mg of ibuprofen (Brufen®) and 1g of paracetamol. Opioid medications (Codeine and Morphine) should be avoided as they cause constipation.
You should follow up with your colorectal surgeon in 6 weeks to review your wound and discuss further management if indicated.